Understanding the Motor End Plate: The Key to Muscle Function
Table of Contents
- What I Mean by “Motor End Plate” and Why It Matters
- The Neuromuscular Junction in Context
- Three key parts you’ll see in every diagram
- Anatomy and Microstructure of the Motor End Plate
- Junctional folds and surface area
- Receptors, enzymes, and the basal lamina
- The clustering story: Agrin, MuSK, and Rapsyn
- Mitochondria and local support
- How the Motor End Plate Turns a Nerve Signal into Muscle Movement
- Step-by-step transmission at the NMJ
- Ions, depolarization, and the all-or-none principle
- Safety factor and what it buys you
- “Which Structure Is Highlighted?” How I Identify the Motor End Plate in Images
- Light microscopy vs electron microscopy
- Stains and labels that make the NMJ pop
- Quick checks I use in labs and exams
- Clinical Relevance: Disorders and Toxins That Target the NMJ
- Myasthenia gravis
- Lambert-Eaton myasthenic syndrome
- Botulism and tetanus
- Organophosphates, curare, alpha-bungarotoxin, and neuromuscular blockers
- Myasthenic crisis vs cholinergic crisis
- Congenital myasthenic syndromes
- Testing and Diagnosis: EMG, Repetitive Nerve Stimulation, and More
- Practical Tips, Analogies, and Study Guides That Helped Me
- Conclusion: Why the Motor End Plate Deserves a Spot on Your Mental “Must Know” List
What I Mean by “Motor End Plate” and Why It Matters
When I first learned the term “motor end plate,” I kept mixing it up with the whole neuromuscular junction. I don’t do that now. The motor end plate is the specialized bit of the muscle fiber’s membrane—the sarcolemma—that sits right under the nerve terminal. That spot forms the postsynaptic membrane in the neuromuscular junction. Think of it as the receiving dock on the muscle side. The motor neuron ships acetylcholine. The motor end plate signs for the delivery, opens the door, and kicks off muscle contraction.
If your question is “Which structure is highlighted—motor end plate?” you’re usually looking at the folded region of the muscle cell membrane right beneath the presynaptic terminal. It’s the postsynaptic component of the NMJ. That region is packed with nicotinic acetylcholine receptors (nAChRs) and shaped into deep junctional folds that boost the signal. I like calling it the muscle’s welcome mat for the nerve.
The Neuromuscular Junction in Context
To see the motor end plate clearly, you need to zoom out for a second. The neuromuscular junction (NMJ) is where a motor neuron talks to a skeletal muscle fiber. This is a chemical synapse. Not an electrical synapse. Chemical means neurotransmitter release across a synaptic cleft and receptor binding on the other side.
Three key parts you’ll see in every diagram
- Presynaptic terminal (axon terminal of a motor neuron)
- This terminal bouton holds synaptic vesicles, active zones, and voltage-gated calcium channels.
- Synaptic cleft
- The tiny gap that includes a basal lamina filled with acetylcholinesterase.
- Motor end plate (the postsynaptic membrane of the muscle fiber)
- The sarcolemma with junctional folds and dense clusters of nAChRs.
That trio makes up the core of skeletal muscle innervation in the somatic nervous system. The motor neuron drives a motor unit. Each motor unit branches to several muscle fibers. Each fiber receives input from a single motor neuron at one primary endplate region under normal conditions.
Anatomy and Microstructure of the Motor End Plate
Junctional folds and surface area
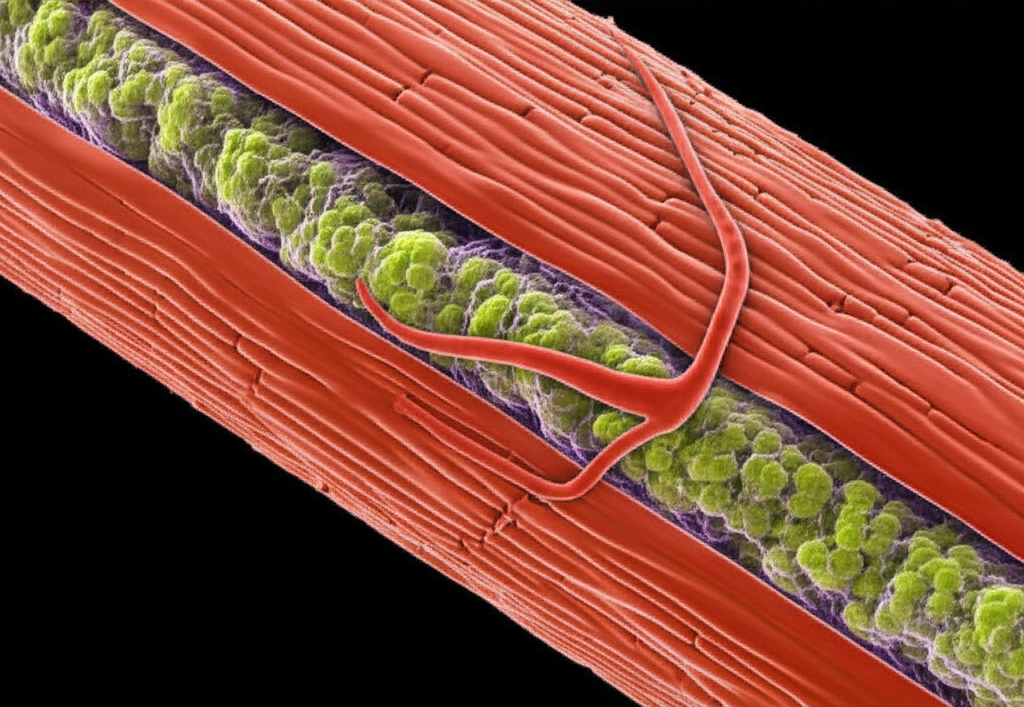
The motor end plate isn’t smooth. It dives into deep junctional folds. Those folds increase surface area. More area means more receptors. More receptors means a stronger response. When I first saw electron microscopy images of these folds, the pattern looked like a comb pushed into clay.
You’ll see nAChRs concentrated at the crests of the folds. Voltage-gated sodium channels cluster deeper along the sides of the folds. That micro-organization helps drive a strong endplate potential and then trigger an action potential in the surrounding sarcolemma.
Receptors, enzymes, and the basal lamina
Here’s the roll call of the usual suspects:
- Nicotinic acetylcholine receptors (nAChRs)
- Ligand-gated ion channels that open fast when ACh binds.
- Acetylcholinesterase (AChE)
- The enzyme that breaks down acetylcholine in the synaptic cleft. Most of it sits tethered in the basal lamina right opposite the motor end plate.
- Basal lamina
- A specialized matrix between nerve terminal and muscle fiber. It supports alignment. It holds AChE. It guides reinnervation if the nerve gets injured.
Quantitatively, typical adult human motor end plates hold roughly 1 to 2 million AChRs clustered at those crests. Each open receptor allows a gush of sodium ions in the millisecond range. That surge kicks off a local depolarization. The motor end plate is very good at its job.
The clustering story: Agrin, MuSK, and Rapsyn
A neuron-derived protein called agrin helps set the stage. Agrin interacts with the LRP4/MuSK receptor complex on the muscle side. That signal recruits rapsyn, the scaffolding protein that clusters AChRs at the motor end plate. If you knock out parts of this pathway in congenital myasthenic syndromes, you lose proper receptor aggregation. Transmission drops. Weakness follows.
Mitochondria and local support
You’ll find a high density of mitochondria in the region. Why. There’s a lot of upkeep. Receptors cycle. Proteins turn over. Ion pumps work. The postsynaptic density anchors structural proteins that keep this zone tight, including links to the cytoskeleton. Dystrophin and related complexes keep the membrane stable during contraction. Schwann cells cap the presynaptic terminal for protection and support.
How the Motor End Plate Turns a Nerve Signal into Muscle Movement
I love walking through the sequence. It reads like a crisp relay race.
Step-by-step transmission at the NMJ
1) A nerve impulse—an action potential—travels down the motor neuron to the presynaptic terminal.
2) Voltage-gated calcium channels open when the terminal depolarizes. Calcium ions rush in.
3) Calcium triggers synaptic vesicles to fuse at active zones. The vesicles release acetylcholine into the synaptic cleft.
4) Acetylcholine binds to nAChRs on the motor end plate within microseconds.
5) The open receptors allow sodium influx and a smaller potassium efflux. The net current depolarizes the postsynaptic membrane.
6) That depolarization is the endplate potential (EPP). Enough ACh means enough receptors open. The EPP hits threshold.
7) Voltage-gated sodium channels in the muscle membrane fire an action potential along the sarcolemma and down the T-tubules.
8) Excitation-contraction coupling kicks in. Calcium floods from the sarcoplasmic reticulum. The myofilaments slide. Muscle contraction follows.
Even the “noise” matters. When a single vesicle releases its quantum of ACh spontaneously, you get a miniature endplate potential (MEPP) of roughly 0.5 to 1.0 mV. A single nerve impulse usually releases 100 to 200 quanta. The EPP rises to roughly 30 to 50 mV. That sits well above the threshold needed to fire the muscle action potential. That gap gives you a safety factor.
Ions, depolarization, and the all-or-none principle
The motor end plate produces a graded potential. The action potential that follows obeys the all-or-none principle. Cross threshold and the muscle fiber fires. Fall short and it stays quiet. That line in the sand keeps transmission crisp and reliable.
Safety factor and what it buys you
Healthy NMJs have a strong safety factor. The EPP overshoots threshold under normal conditions. You need that cushion. Fatigue sets in. Temperature shifts. Small defects happen. The safety factor gives you headroom. In diseases like myasthenia gravis, the safety factor shrinks. EPP amplitudes drop toward threshold. Some impulses fail. Weakness appears after use.
“Which Structure Is Highlighted?” How I Identify the Motor End Plate in Images
When I tutor students who ask “Which structure is highlighted—motor end plate,” I walk them through a checklist. I start with the big shapes. I finish with fine textures.
Light microscopy vs electron microscopy
- Light microscopy
- On standard stains, you’ll often see the synaptic region as a small, specialized area on the muscle fiber surface. It can be subtle. Fluorescent labels make it obvious. The motor end plate appears where the axon terminal meets the muscle fiber. The folds are hard to resolve with light microscopy alone.
- Electron microscopy
- This is where the magic shows. The presynaptic terminal sits close to the muscle fiber with a narrow synaptic cleft between them. The motor end plate forms the postsynaptic side. It shows deep junctional folds. You’ll see synaptic vesicles docked near presynaptic active zones. The basal lamina fills the cleft and lines the folds.
Stains and labels that make the NMJ pop
Alpha-bungarotoxin binds nAChRs with high specificity. Tag it with a fluorophore and you’ll light up the motor end plate cleanly. Acetylcholinesterase histochemistry marks the cleft and fold region. Combine those with a general axon marker and you get a sharp picture of presynaptic terminal, synaptic cleft, and postsynaptic motor end plate.
Quick checks I use in labs and exams
- Look for the folded postsynaptic membrane on the muscle side.
- Confirm the presynaptic terminal with vesicle clusters.
- Identify the synaptic cleft with a thin, uniform gap.
- Remember: the motor end plate equals the postsynaptic membrane of the muscle fiber at the NMJ. That is the highlight you’re being asked to name.
Clinical Relevance: Disorders and Toxins That Target the NMJ
I work from function-to-failure. If you know each domino, you can find the fallen one.
Myasthenia gravis
Myasthenia gravis (MG) hits the motor end plate directly in most cases. Autoantibodies target and reduce available nicotinic acetylcholine receptors. Roughly 85 to 90% of MG patients show antibodies that block or remove nAChRs. Fewer receptors means smaller EPPs. The safety factor shrinks. Muscles fatigue with use. Weakness fluctuates.
Numbers matter here. MG prevalence runs about 150 to 250 per million worldwide. Repetitive nerve stimulation on EMG often shows a decremental response greater than 10% by the fourth or fifth stimulus in about three-quarters of generalized MG cases. That pattern reflects reduced postsynaptic receptor availability at the motor end plate.
Treatment targets the problem with several tools:
- Pyridostigmine or neostigmine inhibit AChE. More ACh hangs around the cleft for longer.
- Immunosuppressants help reduce antibody production.
- Thymectomy helps in selected cases.
- Rescue therapies step in for myasthenic crisis.
Lambert-Eaton myasthenic syndrome
LEMS attacks the presynaptic side. Autoantibodies target the presynaptic voltage-gated calcium channels. Reduced calcium influx means fewer vesicles release ACh. The motor end plate becomes under-stimulated even though its receptors may be fine. LEMS remains rare with a prevalence near 0.4 per million. Repetitive nerve stimulation can show facilitation at high frequencies or after maximal voluntary contraction. The extra stimulation boosts residual release. EPPs rise. The clinical weakness improves briefly after effort.
Botulism and tetanus
Botulism blocks ACh release by cleaving SNARE proteins inside the presynaptic terminal. The motor end plate sits ready with receptors. No signal arrives. Flaccid paralysis follows. The pattern often starts with cranial nerves and descends. Tetanus works differently. The toxin blocks inhibitory interneurons in the central nervous system. That loss of inhibition produces spastic paralysis. The NMJ keeps releasing ACh normally in tetanus.
Organophosphates, curare, alpha-bungarotoxin, and neuromuscular blockers
Organophosphate poisoning knocks out acetylcholinesterase. ACh lingers in the cleft. The motor end plate faces a flood. Receptors overstimulate then desensitize. The result looks like weakness with fasciculations and cholinergic signs. Curare-like agents act as competitive antagonists at the nAChR. Alpha-bungarotoxin binds nAChRs tightly as well. Anesthesiologists use neuromuscular blocking agents to control paralysis during surgery. Those agents target the NMJ in specific ways. Depolarizing blockers like succinylcholine hold the gate open briefly then desensitize it. Nondepolarizing agents like rocuronium compete at the receptor.
Myasthenic crisis vs cholinergic crisis
I separate these in my head with a simple rule. Myasthenic crisis happens when receptor availability drops too low. Cholinergic crisis happens when ACh builds up too much because of AChE inhibition. Both present with weakness. Pupils and secretions give you clinical clues. The treatment pathways diverge.
Congenital myasthenic syndromes
Congenital myasthenic syndromes (CMS) present a diverse picture. Dozens of genes can be involved. Some hit AChR subunits. Others target AChE or proteins involved in receptor clustering like MuSK or rapsyn. The end result is inefficient synaptic transmission at the motor end plate. Kids may present with fatigable weakness early in life. The details depend on which step falters.
Testing and Diagnosis: EMG, Repetitive Nerve Stimulation, and More
Electromyography and nerve conduction studies give you windows into the neuromuscular junction. RNS-EMG looks at compound muscle action potentials during repeated stimulation.
- In MG, you see a decrement over several stimuli because postsynaptic receptor numbers run low.
- In LEMS, high frequency stimulation or brief maximum effort produces an incremental response. Presynaptic calcium builds up. ACh release improves for a moment. The motor end plate finally gets more to work with.
Single-fiber EMG can detect jitter and blocking. That test reaches for fine-grained disruption in neuromuscular transmission. Put those results alongside clinical patterns and antibody tests. You’ll have a strong diagnostic picture.
Practical Tips, Analogies, and Study Guides That Helped Me
I like to anchor neurophysiology with analogies. The NMJ works as a one-to-one high-fidelity synapse. The goal is reliable transmission from nerve impulse to muscle action. That design reminds me of engineered systems that value predictable power transfer.
- Think about the motor end plate like the stator face in an electric motor. The nerve terminal plays like a rotor delivering the changing field. The analogy is not literal. It helps me picture matched surfaces built for transfer. If the comparison helps you too, you might enjoy a quick refresher on the stator and rotor relationship in electromechanics.
- Junctional folds boost surface area the way laminations and stacking patterns boost performance in electric machines. Again, not the same physics. The mental model still helps. If you like peeking at manufacturing tricks that squeeze out efficiency, this overview of electrical steel laminations can scratch that itch.
- The safety factor at the NMJ feels like a design margin that engineers bake into systems. More than enough ACh and receptors to cross threshold under stress. That echoes the way designers think about headroom with load and resistance. You can revisit the basics with this concise guide to motor principle.
Beyond analogies, here are practical nuggets that have stuck with me:
- Chemical vs electrical synapse
The NMJ is chemical. Neurotransmitter crosses a cleft. Electrical synapses use gap junctions to pass current directly. This distinction clarifies why we talk about vesicles, receptors, and a synaptic cleft.
- Endplate potential vs EPSP
The EPP is a specialized excitatory postsynaptic potential at the NMJ. It’s big. It’s graded. It almost always crosses threshold in healthy muscle because of the safety factor.
- Denervation and reinnervation
After denervation, AChRs spread beyond the endplate. The muscle becomes denervation hypersensitive. Reinnervation pulls the receptors back into a tight cluster at the motor end plate.
- Strength comes from reliability
The NMJ’s reliability stems from the all-or-none principle and the safety factor. The design ensures that one nerve spike triggers one muscle fiber spike. That gives you precise control.
When I study pathology, I map each disease to the step it breaks:
- Receptor loss at the postsynaptic site: MG.
- Presynaptic calcium channel block: LEMS.
- Vesicle fusion failure: botulism.
- Enzyme block in cleft: organophosphates.
- Competitive antagonism at the receptor: curare-like agents.
- Excess ACh due to enzyme inhibition: cholinergic crisis.
I jot ions in the margin too:
- Calcium influx at the presynaptic terminal triggers release.
- Sodium influx at the motor end plate drives depolarization.
- Potassium efflux balances the currents and helps repolarization.
If you love mechanical metaphors during review, one more advanced analogy can help you picture how structure supports function. In electric machines, designers use endplates and laminations to shape magnetic paths and manage losses. The biology is different. The design theme rhymes. Surface area, alignment, and robust margins boost reliability. If you want a visual of how laminated stacks look in a stator core, this quick tour of stator core lamination illustrates how layered structure enables performance.
Conclusion: Why the Motor End Plate Deserves a Spot on Your Mental “Must Know” List
Here’s what I want you to carry forward. The motor end plate is the postsynaptic face of the neuromuscular junction. It’s a specialized region of the muscle fiber membrane built for high-fidelity transmission. Junctional folds multiply surface area. Nicotinic acetylcholine receptors cluster at the crests. Acetylcholinesterase in the basal lamina keeps the signal short and sharp. Mitochondria support the heavy metabolic load. The whole setup produces a robust endplate potential that overshoots threshold and fires a muscle action potential. That chain of events pulls calcium out of the sarcoplasmic reticulum and makes the muscle contract.
In clinics and in the lab, I look for breakdowns at each step. Myasthenia gravis shrinks the safety factor by cutting receptors. Lambert-Eaton starves the cleft by throttling calcium channels in the presynaptic terminal. Botulism jams vesicle fusion. Organophosphates paralyze the cleft’s cleanup crew. Congenital myasthenic syndromes disrupt assembly by targeting agrin, MuSK, rapsyn, or receptor subunits. EMG and repetitive nerve stimulation reveal those failures through predictable patterns.
If your screen shows a labeled diagram and you ask “Which structure is highlighted—motor end plate,” look for the folded postsynaptic membrane on the muscle fiber right opposite the axon terminal. That is the receiving dock that turns acetylcholine into an endplate potential. That potential crosses threshold and sends the muscle on its way to contraction. The design is elegant. The purpose is clear. The more I study it, the more I appreciate how much depends on those tiny folds and crowded receptors.
Before I wrap up, one last analogy for the visual thinkers. Biological and engineered systems both lean on clear principles and thoughtful structure. Electric motors pin torque on field interactions and geometry. Muscles pin force on calcium and proteins. Both rely on clean handoffs at critical interfaces. If you enjoy seeing how interfaces drive performance in machines, you might like this short read on the relationship between stator and rotor. It pairs well with a final mental picture of the motor end plate: a compact, beautifully tuned interface that turns nerve intent into movement you can feel.
Key terms you met here include neuromuscular junction, motor neuron, muscle fiber, synaptic cleft, acetylcholine receptors, presynaptic terminal, postsynaptic membrane, action potential, synaptic vesicles, voltage-gated calcium channels, junctional folds, basal lamina, acetylcholinesterase, endplate potential, miniature endplate potential, agrin, MuSK, rapsyn, motor unit, Schwann cell, excitation-contraction coupling, safety factor, denervation hypersensitivity, and more. You now know what to look for, how it works, and why it matters when health falters.
If you keep these mental anchors handy, your next slide or exam question about the motor end plate will feel like a friendly face rather than a curveball.