What is Motor Planning? Understanding Praxis, Challenges & How to Improve It
Table of Contents
- Introduction: The unseen architect of everyday movement
- Defining motor planning: Beyond simple movement
- The three pillars of praxis: Ideation, planning/sequencing, execution
- Motor planning vs motor control vs motor learning
- How planned movements become automatic
- The brain’s blueprint: Neuroscience of motor planning
- Key brain regions and what they do
- Sensory systems that guide planning
- Feedforward vs feedback control and motor programs
- Why motor planning matters for life skills
- Child development milestones
- Daily living skills
- Learning and academics
- Social participation and complex skills
- Recognizing challenges: Signs of motor planning difficulties
- Dyspraxia, apraxia, and related terms
- Indicators across ages
- Associated conditions: ASD, ADHD, SPD
- How we assess motor planning
- Observation and functional tasks
- Standardized tools and what they tell us
- Empowering movement: Strategies and interventions that work
- Professional support: OT, PT, SLP
- Practical home and school strategies
- Sensory-rich activities and “heavy work”
- Bilateral coordination, crossing midline, and core strength
- Sports, music, and play as therapy
- Advanced insight: Theories that shape practice
- Schema theory, dynamic systems, degrees of freedom
- Embodied cognition, mirror neurons, and motor imagery
- Special focus: Oral motor planning and speech
- Developmental apraxia of speech and verbal dyspraxia
- How SLPs approach treatment
- Motor planning across the lifespan
- Infants and toddlers
- School-age kids and teens
- Adults
- Hope and progress: Neuroplasticity in action
- Quick detour: If you meant electric motors
- Conclusion: A foundation for independence and confidence
Introduction: The unseen architect of everyday movement
I still remember a little boy I’ll call Liam who froze at the top of a playground ladder. He had the strength to climb. He’d seen other kids do it. He wanted it. What he lacked wasn’t muscle or motivation. He didn’t know how to put the steps together in his body. That moment changed how I think about movement. Motor planning isn’t a luxury skill. It’s the unseen architect of everyday action.
You use motor planning when you tie your shoes, ride a bike, copy a yoga pose, or learn a new dance. Kids need it for play and school. Adults need it for work and daily living. When motor planning falters, life gets harder. I’ve watched kids labeled “clumsy” blossom when we address praxis directly. I’ve also watched adults rebuild complex skills after brain injury through focused practice. In this guide I’ll share what motor planning is, why it matters, how the brain does it, what goes wrong, and what you can do to help.
Defining motor planning: Beyond simple movement
Here’s the core definition I use. Motor planning, also called praxis, is the cognitive process of conceiving, organizing, and executing an unfamiliar motor action efficiently. That “unfamiliar” piece matters. You don’t plan each finger twitch when you type a familiar password. You do plan when you learn a new knot, dribble a basketball for the first time, or figure out a tricky zipper.
The three pillars of praxis: Ideation, planning/sequencing, execution
I like to break praxis into three stages:
- Ideation: What to do. This is the spark. “I’ll climb over that log” or “I’ll scoop sand then pour it into the bucket.” Kids with ideation challenges struggle to come up with novel actions during play. They repeat the same moves or wait for someone to tell them what to do.
- Motor planning and sequencing: How to do it. You organize steps, anticipate the feel of movement, and sequence motor movements. You use working memory and visuospatial skills to figure out positions in space. You tap body awareness and proprioception to set force and timing. This is where feedforward control sets a plan before you move.
- Motor execution: Do it. Your muscles fire. Postural control keeps you steady. Your cerebellum fine-tunes timing. Feedback control uses sensory input to adjust on the fly.
Motor planning vs motor control vs motor learning
People mix these terms. I separate them like this:
- Motor planning: Conceiving and sequencing a novel action before and during movement.
- Motor control: Regulating movement once it starts. Think balance, coordination, force modulation, and postural control.
- Motor learning: The process that turns clumsy first tries into smooth, automatic movement over time. Practice and feedback build generalized motor programs you can reuse across contexts.
How planned movements become automatic
You plan a movement the first few times. With repetition you need less conscious effort. The basal ganglia help shift actions from planned to habitual. The cerebellum refines timing and error correction. Over time you store generalized motor programs that handle similar actions with small tweaks. That’s how you can learn to button one shirt and then manage a different shirt without starting from scratch.
The brain’s blueprint: Neuroscience of motor planning
Key brain regions and what they do
- Frontal lobe: Sets goals and holds the plan in mind. Executive functions like working memory, inhibition, and cognitive flexibility shape how well you plan.
- Premotor cortex and supplementary motor area: Prepare and sequence actions. The SMA helps with bimanual coordination and internally generated sequences.
- Motor cortex: Sends the primary commands to muscles.
- Parietal lobe: Builds body schema and spatial awareness. It integrates sensory information so the plan suits your body in space.
- Basal ganglia: Initiate movement and chunk sequences into habits. They play a role in sequencing and action selection.
- Cerebellum: Handles timing, precision, and error correction. It compares expected and actual feedback.
- Thalamus: Acts as a relay that helps sensory and motor information communicate efficiently.
Sensory systems that guide planning
Motor planning depends on accurate sensory input:
- Proprioception: Your sense of body position and force. It tells you how much to push or pull.
- Vestibular system: Your sense of balance and head movement. It sets the stage for postural control and stable gaze.
- Vision: Guides hand and foot placement and helps with visuospatial mapping.
- Tactile input: Informs grip, texture handling, and safety.
When proprioceptive or vestibular input runs noisy or low, kids may look clumsy. They overshoot or undershoot. They lose balance on turns. They avoid swings or seek deep pressure. Sensory processing and motor planning go hand in hand.
Feedforward vs feedback control and motor programs
Planning uses feedforward control. You predict the feel of movement and set a plan. As you move you use feedback control to correct errors. If you pour water and see it miss the cup, you adjust your wrist midpour.
Over time you build generalized motor programs. These are flexible templates that handle categories of actions. You don’t program every muscle fiber. You store core patterns then adapt parameters like force and speed. The “degrees of freedom problem” describes how your brain manages the countless ways to move a limb. Your nervous system simplifies options by coupling joints and using synergies.
Why motor planning matters for life skills
Child development milestones
Motor planning drives early milestones:
- Infants: Rolling, reaching across midline, bringing hands to mouth.
- Toddlers: Walking, climbing, stacking blocks, simple tool use.
- Preschoolers: Hopping, galloping, drawing basic shapes, using two hands together.
- School-age: Riding a bike, handwriting, keyboarding, sports drills.
Activities of daily living
You need motor planning for:
- Dressing: Sequencing pants on first, then socks, managing buttons and zippers.
- Eating: Coordinating utensils and cup control.
- Hygiene: Toothbrushing with consistent force and a full-mouth sequence.
- Handwriting: Coordinating grip, pressure, letter formation, and visual-motor integration.
Academic and learning skills
The impact shows up in classrooms:
- Cutting on lines, using rulers, managing binders and backpacks.
- Writing and revising written work without fatigue.
- Participating in physical education and playground games.
Social participation and complex skills
Motor planning supports coordinated play and non-verbal communication. Think gestures, body language, group games, or team sports. It also supports complex skills like musical instruments, crafts, woodworking, and coding with robotics kits where hand control matters.
Recognizing challenges: Signs of motor planning difficulties
Dyspraxia, apraxia, and related terms
- Dyspraxia or Developmental Coordination Disorder (DCD): A developmental condition marked by difficulties in learning or performing coordinated motor skills. Prevalence is often cited around 5–6% of school-aged children. Some estimates go higher for milder forms.
- Apraxia: A difficulty with planning and executing purposeful movements that isn’t explained by weakness or comprehension problems. It can be acquired after brain injury or stroke.
- Verbal dyspraxia or Developmental Apraxia of Speech (DAS): A childhood speech motor planning disorder. Kids know what they want to say but can’t plan the sound sequences reliably.
Different types of apraxia include ideational apraxia, ideomotor apraxia, limb-kinetic apraxia, constructional apraxia, oral apraxia, and verbal apraxia. The names point to which stage or skill breaks down.
Indicators across ages
Common signs I watch for in children and adults:
- Frequent clumsiness, tripping, bumping into objects.
- Difficulty learning new motor skills or imitating postures.
- Trouble with multi-step tasks like getting dressed or packing a bag.
- Appearing awkward, uncoordinated, or slow to respond when a new task is presented.
- Poor body awareness or spatial awareness. People feel lost in their own bodies.
- Weak postural control with fatigue during desk work.
- Reluctance to join motor tasks due to frustration.
- For speech: Inconsistent sound production, disrupted prosody, and visible effort in planning syllables.
Associated conditions: ASD, ADHD, SPD
You can see motor planning challenges within Autism Spectrum Disorder. Research reports distinct issues with imitation, gestural praxis, and coordination. ADHD often brings motor control and planning difficulties that affect handwriting and sports. Sensory Processing Disorder can complicate planning when proprioceptive, vestibular, or tactile systems go out of tune. Executive function challenges can make sequencing and working memory harder which impacts motor planning.
How I unpack a confusing picture
Two children can look “clumsy” for very different reasons. One child struggles to plan. Another has weak core strength and poor balance. A third misreads sensory input. Often I see a mix. So I look at ideation, sequencing, execution, and sensory contributions rather than using a single label.
How we assess motor planning
Observation and functional tasks
I start with simple, real tasks. Can the child copy a multistep obstacle course. Can an adult imitate three yoga poses in sequence. Can they plan transitions between floor and standing without prompts. I also note bilateral coordination and crossing the midline. I watch how they initiate, how they adapt, and whether they need lots of external cues.
Standardized tools and what they tell us
Professionals may use:
- BOT-2 (Bruininks-Oseretsky Test of Motor Proficiency): Measures fine and gross motor skills like balance, coordination, and manual dexterity.
- DCDQ (Developmental Coordination Disorder Questionnaire): A parent report that screens for DCD.
- Sensory Integration and Praxis Tests (SIPT): A set of tests that dig into sensory processing and praxis. You need specific training to administer it.
- Additional measures may include visual perception, visual-motor integration, and postural control assessments.
If you suspect motor planning challenges, talk with an Occupational Therapist for functional skills, a Physical Therapist for balance and gait, or a Speech-Language Pathologist for speech motor planning. Don’t self-diagnose. A thoughtful evaluation gives you a clear plan.
Empowering movement: Strategies and interventions that work
I’ve watched kids and adults surprise themselves when we pick the right strategies. Here are approaches that deliver.
Professional support: OT, PT, SLP
- Occupational Therapy (OT): OT addresses sensory integration, praxis, hand skills, and activities of daily living. Many OTs use task-specific training, motor learning principles, and sensory-informed approaches. Frameworks like DIR/Floortime can support ideation through playful engagement and co-regulation.
- Physical Therapy (PT): PT builds strength, balance, and coordination. PT targets gait, postural control, and higher-level gross motor planning like agility and change of direction.
- Speech-Language Pathology (SLP): For Developmental Apraxia of Speech and oral motor planning, SLPs use structured, high-repetition approaches with visual and tactile cues.
Practical home and school strategies
- Break tasks down: Chunk dressing into logical, bite-sized steps. Front-load a simple visual sequence. Reduce the cognitive load.
- Model then fade: I demonstrate once. Then I use less cueing each round. I let the child take the lead as soon as possible.
- Use visual supports: Visual schedules, simple diagrams, or key photos help reduce working memory demands.
- Keep instructions clear and concise: One step at a time for new tasks.
- Offer time and repetition: You need practice to build motor learning. Short daily reps beat one long weekend session.
- Celebrate effort and problem-solving: Praise flexible thinking. Don’t wait for perfect execution.
Sensory-rich activities and “heavy work”
A good “sensory diet” supports body awareness which supports planning. Examples:
- Proprioceptive activities: Animal walks, wheelbarrow walks, carrying groceries, pushing a laundry basket, theraband pulls, tug-of-war, play dough and putty.
- Vestibular activities: Swings, scooter boards, log rolls, gentle spinning with control and stops, balance beams, coordinated head turns during walking.
- Tactile activities: Messy play with shaving cream, slime, kinetic sand, finger painting, and sensory bins with rice or beans.
Proprioceptive input tends to calm and organize. Vestibular input needs careful dosing. Start slow and track reactions. Pair vestibular input with grounding heavy work when needed.
Bilateral coordination, crossing midline, and core strength
Bimanual coordination unlocks so many daily skills. Try:
- Clapping patterns then body percussion.
- Ribbon or scarf dances that cross midline.
- Alternating hand dribbles, two-hand toss and catch, and figure-eight ball paths around legs.
- Obstacle courses that force whole-body sequencing with core engagement. Crawl under, climb over, step through, then stop on a spot.
Core strength matters for postural control and frees the hands for fine motor planning. Planks, bear walks, bridges, and tall kneeling play build that base.
Sports, music, and play as therapy
I’ve had great success with:
- Simon Says and copycat games.
- Yoga for kids and adults. Hold poses and transition smoothly to blend planning with execution.
- Dance follow-alongs or short choreography. Start slow then build speed.
- Martial arts patterns for sequencing and control.
- Beginner instrument patterns like simple drum beats. Rhythm supports timing and sequencing.
- “Follow the recipe” cooking for sequencing, safety planning, and tool use.
Advanced insight: Theories that shape practice
You don’t need a PhD to help your child or yourself. Still, a few ideas sharpen your choices.
- Motor learning: Schema theory explains how practice builds generalized motor programs that transfer to new contexts. Vary parameters like force and speed so the brain learns the “rules” of the movement.
- Dynamic systems theory: Movement emerges from the interaction of person, task, and environment. Change one variable to unlock a new pattern. Lower the rim so the shot succeeds then raise it slowly.
- Degrees of freedom problem: The body has many moving parts. We solve it by coupling joints into synergies and chunking actions.
- Embodied cognition: Cognition lives in the body too. Move the body and you engage the brain. I see ideation improve when kids move through space with rich sensory input.
- Mirror neurons and imitation: Watching actions lights up parts of the motor system. Use clear demonstrations and slow motion. Add motor imagery by asking kids to picture themselves doing the move before trying it.
- Feedforward and feedback loops: Plan before you act then tune during action. Provide external feedback early then fade it so internal feedback takes over.
Special focus: Oral motor planning and speech
Motor planning doesn’t stop at limbs. Oral motor planning affects chewing and speech. In Developmental Apraxia of Speech, children know what they want to say yet struggle to plan sound sequences. You hear inconsistent errors and disrupted rhythm. SLPs often use approaches built on high repetition, visual cues, tactile prompts, and careful pacing. Progress can feel slow at first then it snowballs. I cheer small wins because they add up.
Motor planning across the lifespan
Infants and toddlers
I look for early motor planning in play. Reaching and bringing hands together. Trying different ways to get a toy. Crossing midline to grab something. Early signs of trouble might include limited exploration, few new play ideas, or strong avoidance of certain movements. Support can be simple. Show one new way to play with a toy. Offer safe climbing and crawling paths. Narrate the steps.
School-age kids and teens
School amplifies demands. You see issues in handwriting, cutting, PE, and team games. Teens may avoid sports or practical classes that reveal coordination gaps. Build in strengths. Some kids thrive in swimming or track because the rules are clear and the environment is consistent. Others love coding robots or building with LEGO which supports fine motor sequencing and spatial planning.
Adults
Adults with DCD often find workarounds. They may type instead of handwrite. They pick sports that fit their patterns. If a stroke or injury leads to acquired apraxia or limb-kinetic apraxia, targeted neurorehabilitation can restore function. Task-specific practice and principles of neuroplasticity guide recovery. Success depends on intensity, repetition, and meaningful goals.
Hope and progress: Neuroplasticity in action
I’ve watched families light up when a child learns to ride a bike after months of stepwise practice. I’ve watched adults relearn how to make a cup of tea after brain injury using careful task analysis and repetitive practice. The brain changes with use. It needs clear goals, frequent reps, feedback, and just-right challenge. You don’t outgrow the ability to improve. You scaffold it.
Practical programs often combine:
- Task-specific training with graded difficulty.
- External feedback early then internal feedback as skill grows.
- Contextual interference like varied practice to build flexible schemas.
- Rest and recovery to consolidate learning.
Case reflections I keep returning to
- A child who hated shoe tying mastered it after we filmed his hands and added a visual two-step card. He rehearsed the plan in his head first then moved. Motor imagery mattered.
- A teen with ADHD improved handwriting by doing five minutes of heavy work before class and using lined paper with bold margins. Executive function supports eased the planning load.
- A parent who broke down toothbrushing into a three-step visual cue saw less resistance and more independence in two weeks.
These are small stories. They echo what the research says. Early support helps. Task-specific practice works. Family confidence rises when we share clear strategies.
Motor planning in education and learning
Teachers can make a big difference with small tweaks:
- Seat kids with postural needs so their feet land flat. Stable base equals better hand control.
- Use visual schedules and checklists for routines.
- Allow extra time for transitions that require planning.
- Offer alternatives to handwriting when content matters more than penmanship.
- Build motor breaks and proprioceptive “heavy work” into the day. It regulates and prepares the system to learn.
- Teach note-taking structures and typing shortcuts to reduce working memory load.
Therapeutic interventions that often help
- Sensory Integration approaches as developed by Dr. A. Jean Ayres inform many OT sessions though we always pair sensory input with purposeful action.
- DIR/Floortime uses relationship and play to nurture ideation and sequencing.
- Cognitive approaches build self-monitoring and strategy use. “Plan, do, check” routines help kids own the process.
- Sports psychology techniques like visualization and graded exposure apply to motor planning too. Picture the move then try it.
- Therapeutic Listening and other auditory-based supports sit in some programs. I use them when sensory profiles suggest benefit and always with function-based goals.
Special notes on common daily skills
Handwriting
- Focus on grip, posture, and letter formation. Use multisensory tracing, short bursts, and high-contrast guidelines.
Dressing
- Teach one closure at a time. Put a colored dot near a button and a matching dot on the hole to reduce visual search.
Eating
- Work on utensil grip and wrist stability with short-handled spoons and forks. Practice scooping with thicker textures first.
Play
- Use obstacle courses to scaffold sequencing. Start with two steps then add one new piece each session.
Sports
- Teach isolated components before chaining. Dribble slow with eyes on the ball then add a walk then add a jog.
Gait and balance
- Walk narrow lines, step over and around low obstacles, and add head turns to load the vestibular system.
Bimanual coordination
- Stabilize with one hand and manipulate with the other. Tear tape, open containers, and string beads with assistance then fade help.
Crossing the midline
- Play games that place objects on one side and targets on the other. Encourage reaching across with the far hand rather than switching hands.
Visual-motor integration
- Trace large shapes on vertical surfaces. Use mazes, connect-the-dots, and block designs to link vision and action.
Common questions I hear
Is my child just clumsy or is this dyspraxia
Clumsy happens to everyone. Persistent, significant difficulty with new motor tasks and daily living tasks points toward dyspraxia or DCD. A formal assessment clarifies the picture.
Can you outgrow motor planning issues
People improve with practice. Many learn workarounds that serve them well. True DCD usually persists to some degree yet support changes the game.
Does sensory processing disorder cause motor planning problems
Sensory processing and motor planning feed each other. If your body map runs fuzzy, planning gets tougher. Improve body awareness and planning often rises too.
How does ADHD affect motor planning
ADHD challenges working memory and inhibition which motor planning depends on. Kids can learn better strategies. So can adults.
Does autism always include motor planning difficulties
Not always. Many autistic individuals show distinct motor profiles and imitation challenges. Tailored supports help.
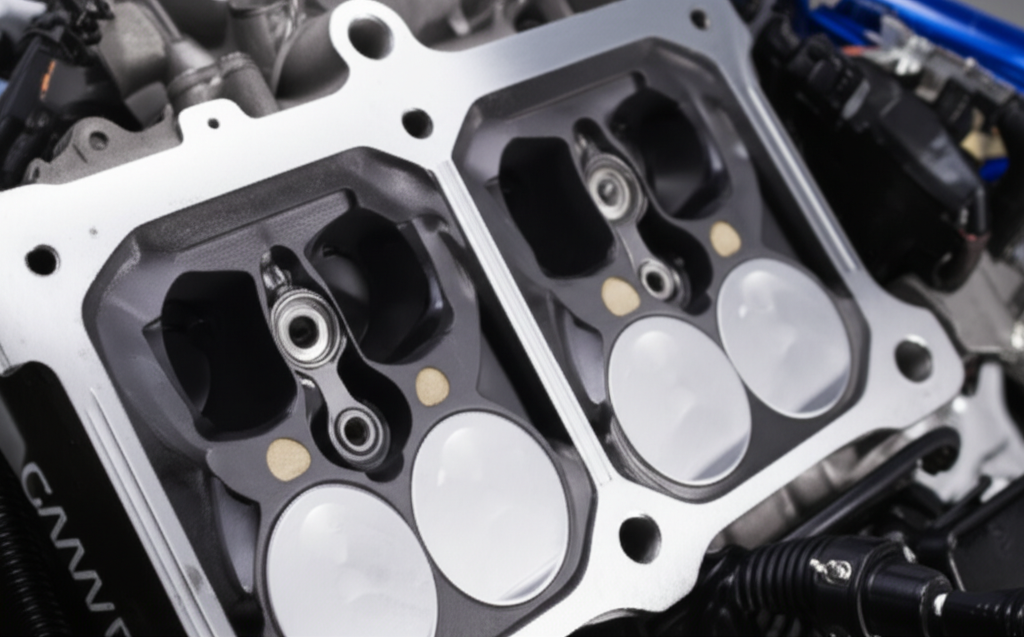
Quick detour: If you meant electric motors
Some readers land on this page looking for the mechanics of electric motors rather than human motor planning. If that’s you, these resources may help:
- A primer on the motor principle
- How stator and rotor work together
- Manufacturing details behind motor core laminations
Conclusion: A foundation for independence and confidence
Motor planning is the quiet power behind every skill we learn. It links ideas to action. It depends on the brain’s planning systems, the body’s senses, and the lessons we store through practice. When it’s hard, life gets noisy. Kids feel clumsy or avoidant. Adults feel frustrated. The good news is simple. You can change the system. You can break steps down. You can dose sensory input to build body awareness. You can practice with purpose.
If you suspect challenges, seek an evaluation with OT, PT, or SLP. Early support helps. Focus on ideation, sequencing, and execution. Use visuals. Use repetition. Praise effort. Start where success can happen then raise the bar one notch at a time. I’ve seen confidence bloom when movement finally makes sense. I bet you will too.
Glossary of key terms at a glance
- Praxis: The process of ideation, motor planning, and execution.
- Ideation: Generating what to do.
- Motor sequencing: Ordering steps in time and space.
- Motor execution: Carrying out the movement.
- DCD/Dyspraxia: Developmental Coordination Disorder with persistent coordination difficulties.
- Apraxia: Difficulty planning purposeful movements often after brain injury. In speech it’s difficulty planning speech sounds.
- Proprioception: Body position and force sense.
- Vestibular system: Balance and head movement sense.
- Visual-motor integration: How vision and movement team up.
- Generalized motor programs: Flexible movement templates built through learning.
- Feedforward control: Plan before moving.
- Feedback control: Correct during movement.
- Crossing the midline: Using one side of the body across the center line.
- Bilateral coordination: Using two hands together in a coordinated way.
- Postural control: Stability that supports skilled movement.
- Sensory diet: A planned set of sensory activities that regulate and prepare the system for function.
Final checklist you can use tomorrow
- Pick one daily task to improve. Break it into three steps.
- Add a visual cue for each step.
- Start with two minutes of proprioceptive “heavy work.”
- Demonstrate once. Let them try. Offer only one cue if stuck.
- Repeat daily for one week. Celebrate small wins.
You just built a simple motor learning plan. Keep going. You’ve got this.
References I keep in mind as I practice
I rely on work from pediatric and rehabilitation fields that show the prevalence of DCD sits around 5–6% in school-aged kids. Meta-analyses report that ADHD often includes motor control and planning deficits that impact handwriting and sports. Systematic reviews of DCD interventions keep pointing to task-specific training and sensory-motor approaches as effective. Cognitive neuroscience continues to link executive functions like working memory and inhibition with motor planning performance. Rehabilitation science keeps proving that targeted, intensive practice leverages neuroplasticity even years after injury. I translate those findings into simple, repeatable steps that families and learners can use in daily life.
Note
This article shares what I’ve learned through years of hands-on work with families, collaboration with Occupational Therapy, Physical Therapy, and Speech-Language Pathology professionals, and ongoing study of motor learning and sensory integration. It is not a diagnosis. For concerns about yourself or a loved one, reach out to a qualified clinician.